Quantifying the Health Impacts of Indoor Particulate Matter
Understanding the human exposome of the indoor environment will place building professionals in the very center of medical and public health work.
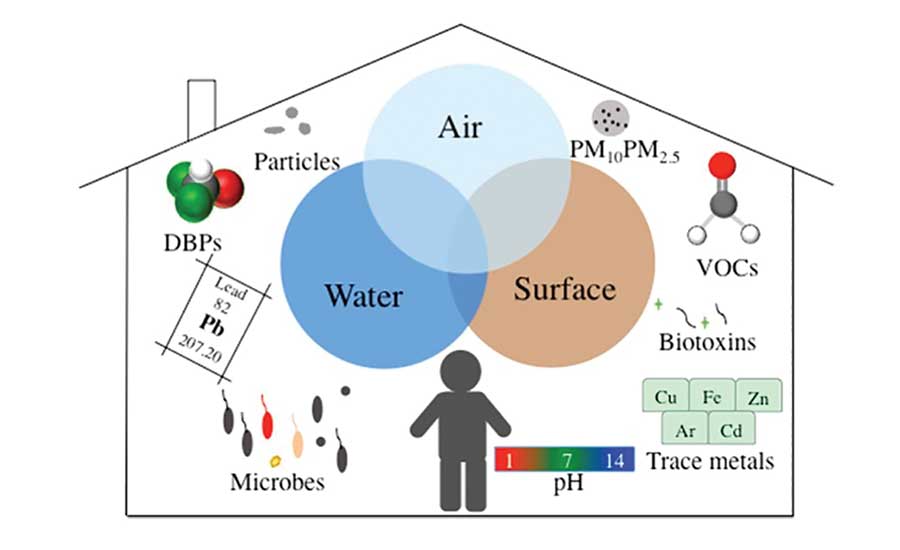
Evidence directly tying the indoor environment to states of health or disease continues to emerge. The relationship between indoor air quality (IAQ) and a wide range of disorders such as infections, autoimmune diseases, allergies, and even cancer is becoming increasingly clear.
Why is this connection coming into focus now? Perhaps it’s because computerized health records allow more comprehensive analysis of disease trends, or HVAC monitoring systems preserve records of IAQ patterns in commercial buildings. Another new set of tools that have dramatically expanded our understanding of the effect of the built environment on our health is the rapid gene sequencing techniques known as metagenomics. These tools have revealed large, diverse, and dynamic communities of bacteria, viruses, and fungi living in and on our bodies. These microbial communities, known as our microbiomes, are our intimate partners and govern almost every aspect of our health. They also respond to conditions in their environment, which is often the same building occupied by humans.
According to the World Health Organization, air pollution caused more than 7 million deaths worldwide in 2012. Of all the air pollutants known to be harmful to our health, fine particulate matter (PM) with diameters of 2.5 microns and smaller is causing the most widespread disease.
The lung is the organ most directly and obviously impacted by inhalation of PM. Fine PM hastens the development of chronic obstructive pulmonary disease, asthma, and lung cancer. Pathology is caused by cascading mechanisms of disease, and once a lung is damaged, it’s very hard to recover full pulmonary function. Beyond the lungs, airborne PM triggers heart attacks, irregular heartbeats, and even disorders like inflammatory bowel disease (IBD). Our digestive system is affected when inhaled PM is cleared from our airways and then swallowed. A person living in urban North America ingests approximately 10^12-10^14 inhaled particles per day. High PM levels are associated with IBD due to changes such as increased gut permeability, decreased colon motility, and alterations in the gut microbiome. In fact, these particles are classified as Group 1 carcinogens because they can trigger the growth of deadly cancers.
Questions such as which airborne particles most easily enter the human respiratory system, how likely it is that inhaled particles may reach the lung, how rapidly they are cleared, and how retained particles will affect the host have been the topics of pulmonology research and treatment. These same questions are now important considerations for the engineer or building manager who chooses and operates HVAC systems.
The best metrics to guide HVAC design would include PM levels generated by indoor activities as well as infiltration of outdoor particles. Unfortunately, this information is very hard to collect because of variations in indoor generation. Consequently, the air pollution measurements that establish HVAC design parameters for filtration and ventilation rates in a given locale come largely from outdoor monitoring.
While outdoor conditions are a good starting point, they do not reflect the most important exposure — that of the indoor environment. Studies in air toxicology show that indoor and outdoor levels of air pollutants can vary widely depending on the compound and the difference between indoor and outdoor temperature and humidity conditions. This disconnect is reflected in hospital statistics, where the increase in hospital admissions for respiratory disease per 10 micrograms per cubic meter increase in outdoor PM2.5 was smaller in the Southwestern U.S. than in the Northeast.
Given the current difficulty in gathering data on indoor exposure to PM, using outdoor data is our only choice. Thankfully, however, on the horizon are small, personal, wearable monitoring devices that will offer more specific information regarding the chemical pollutants, PM size and concentration, and microbial content of the air we breathe and ingest. Understanding the human exposome of the indoor environment will place building professionals in the very center of medical and public health work.
Now that research is clarifying the connection between the indoor environment and our health, we have both an opportunity and a responsibility to rethink how we design and operate our buildings.