Lessons from Unspeakable Tragedies
The recently publicized reports of children dying from Aspergillus fungal infections once again brings into question the culture around reporting errors in U.S. hospitals. Twenty years ago, the Institute of Medicine broke the silence about the epidemic of patient harm from medical errors in health care facilities. The report, “To Err is Human: Building a Safer Health System,” estimated that 98,000 patients died annually from avoidable harm caused by medical errors. Despite the horror of this figure, hospitals still struggle to learn from such near mistakes. Financial penalties from the government, patient and family lawsuits, fear of job loss, psychological constructs of clinicians, and a culture of blame make candid root cause analysis of steps leading up to patient injury almost impossible. Despite these difficulties, the status quo of silence around unintended harm in medicine has to stop. This can only be done by looking at facts and collecting and analyzing data on the underlying dynamics in hospitals.
In this case, two important issues have been raised.
The first obvious reminder is that the hospital building has a powerful impact on patient outcomes and that clinicians and facility managers have to learn to work together with mutual respect.
The second issue is a misunderstanding about moisture management in buildings. Incorrect, or incomplete, thinking about this resulted in hospital building standards lowering the minimum allowable relative humidity (RH) level in operating rooms (ORs) several years ago for reasons having nothing to do with patient safety. In fact, the changes were made to improve the comfort of surgeons and to decrease energy consumption by mechanical systems serving operating suites. While these are important, we are now seeing an alarming increase in surgical site infections around the country.
Moisture management is difficult, especially in cold wintertime climates. Similar to a diet – eating too much or too little food is harmful yet staying in a healthy middle range is challenging. To complicate moisture management even more, many people confuse the side effects of liquid water with those of water vapor or humidity. Despite the difficulties, we must understand and manage moisture correctly because the health consequences of wrong thinking are too severe.
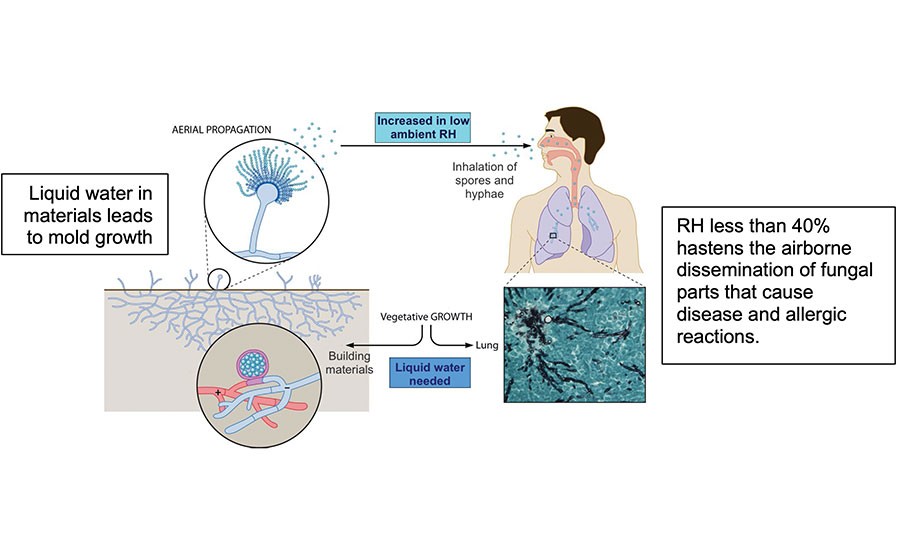
The relationships between indoor fungal communities (mold), water, and occupant allergies or infections is not straightforward. Excess liquid water in building materials clearly contributes to fungal growth, so building professionals try to lower indoor moisture levels as much as possible. The danger to humans is that low ambient RH increases the transmission of dangerous microbes and fungal parts. Even worse, low indoor RH also damages our immunity, the very system that should be protecting us from infections. Clearly, understanding the ins and outs of moisture management is critical in hospitals.
What are the facts? Research from the early 1900s to today show that fungi do not use water vapor for growth. They need liquid water. Of course, in a poorly insulated building, the dew point might be reached near thermal channels or cold pipes. The solution to this is proper insulation, not dry air.
Recent research shows that dry indoor air, or RH less than 40%, is associated with increased illnesses due to at least three factors.
Dry air impairs the human immune system;
Dry air increases the transmission and infectivity of many viruses and bacteria;
When mold is already present on indoor surfaces, lowering RH allows fungal parts and spores to aerosolize and become inhaled by patients and other building occupants.
The data guides us to use HEPA filtration; however, this alone is not adequate. A systematic review on the influence of HEPA filters in units with immunosuppressed patients concluded that while these filters could be occasionally beneficial for patients, a significant decrease in fungal-related mortality rates was not found (as referenced in the graphic atop this column).
Some hospitals are employing germicidal lights in the air ducts. While this sounds promising in the short term, we need more research on the long-term possibility of microbes developing resistance to these light wavelengths. An essential step in the management of indoor air for human health is maintaining a RH 40%-60%. This requires proper building insulation to avoid high water activity in materials, the purchase of safe and effective humidification systems, and regular maintenance of these systems.
Would you take these steps to protect your family? I would.

